Our campaign has officially ended! Still want to make an impact?
To make a contribution, please contact the Development Office at 713-500-3200 or giving@uth.tmc.edu.
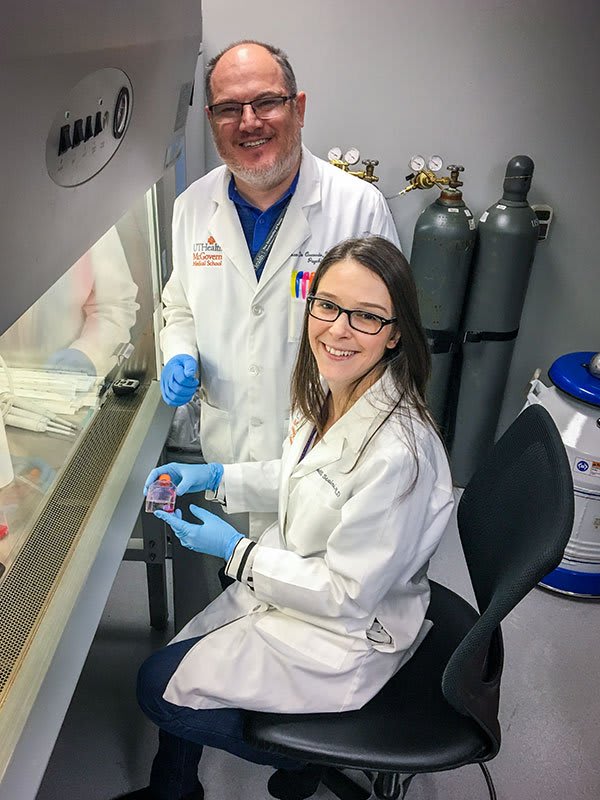
Using extracellular vesicles to study bipolar disorder
In the search for ways to better understand bipolar disorder and develop better treatment for patients, researchers around the world have been focused on the investigation of so-called “biomarkers”. These biological markers can be measured in living patients and be informative of the disease and its processes. However, years of research have led to the discovery of several blood-based biomarkers with very limited clinical use. Their lack of clinical relevance might be related to the fact that most of these blood measurements do not reflect what is actually happening in the brain. Since the assessment of brain biomarkers in living subjects is still quite limited (and brain biopsies are obviously not a possibility), researchers from the Translational Psychiatry Program at the University of Texas Health Science Center at Houston (UTHealth) are studying brain-derived extracellular vesicles that are released in the bloodstream and can be assessed in living patients with bipolar disorder. These vesicles are thought to contain brain-specific information and may thus act as a “peripheral window for the brain” [1]. Specifically, they are known to carry great amounts of non-coding RNAs, including microRNAs, which are thought to play important roles in the pathophysiology of bipolar disorder [2,3] and other neuropsychiatric disorders. This innovative study has been recently funded by the National Institutes of Mental Health (1R21MH117636-01A1), with Dr. Joao Quevedo as Principal Investigator. Co-Investigators also include Dr. Jair C. Soares, Dr. Gabriel R. Fries, Dr. Benson M. Irungu, and Dr. Wei Zhang from the Department of Psychiatry and Behavioral Sciences, Dr. Amit Srivastava from the Department of Pediatric Surgery, and Dr. Zhongming Zhao from the School of Biomedical Informatics. More information on the funded study can be found here.
References
[1] Fries GR, Quevedo J. Exosomal MicroRNAs as Potential Biomarkers in Neuropsychiatric Disorders. Methods Mol Biol. 2018;1733:79-85.
[2] Fries GR, Carvalho AF, Quevedo J. The miRNome of bipolar disorder. J Affect Disord. 2018;233:110-116.
[3] Fries GR, Lima CNC, Valvassori SS, Zunta-Soares G, Soares JC, Quevedo J. Preliminary investigation of peripheral extracellular vesicles' microRNAs in bipolar disorder. J Affect Disord. 2019;255:10-14.
ADHD vs. Bipolar: Diagnosing the Difference in Kids
Diagnosing behavioral conditions can be challenging, especially in kids. Consulting a specialist with a trained eye, who follows best practices for sifting through the symptoms, can make all the difference in obtaining a correct diagnosis—and treating the condition appropriately. Studies estimate that 40-80% of children with bipolar disorder also have Attention-Deficit Hyperactivity Disorder (ADHD). In contrast, 11-20% of kids with ADHD have bipolar disorder. Among children with a mental or behavioral disorder, different behaviors can indicate very different conditions. “These mental health problems in children seem to surface most at school when children are with their same-age peers. They can become distressed by school demands, worsening their mood symptoms,” explains Dr. Zeni, a pediatric psychiatrist and faculty member at UTHealth Department of Psychiatry and Behavioral Health. He reminds caregivers: “When children can’t verbally explain what’s happening, they can express themselves in different ways of acting out.” For example, a child may experience anxious thoughts and express it nonverbally by displaying excessive agitation, which can be confused for hyperactivity. Children may also show unspecific symptoms. For example, irritation or temper outbursts may indicate that something more is happening than frustration; a child may be experiencing manic, depressive or psychotic symptoms. And while some standardized psychological assessments exist, including scales that help differentiate various conditions, a single, comprehensive test does not exist for testing the entire spectrum of possible conditions in children. The spectrum of issues in children is broad. At one end, it can include bipolar disorder or may include intermediate bipolar, where symptoms present for different durations. On the other end of the spectrum, tantrums and outbursts may show up as severe emotions, or mood- dysregulation, with frequent short outbreaks that are disproportional to their cause: Behavior that is currently not associated with bipolar disorder. For pediatric psychiatrists and psychologists, getting to know a child during a single visit is challenging. To obtain clearer information about a child’s condition, a skilled child psychiatrist or psychologist requires more time and also seeks input from parents and from school, where children spend a large portion of their time. Not all problems occur at school. “If a child’s problems are happening everywhere, are basically pervasive,” adds Dr. Zeni, “we can focus on addressing a specific diagnosis, conditions, and treatments.” Psychiatrists review the trajectory of a child’s life to help identify issues that may have occurred earlier in development. Conditions that are not linked to a brain disorder do not always respond to medication, such as family violence, neglect, or unstructured environments. In those cases, a more psychological approach may help address issues. Meanwhile, it is crucial to remain aware that children are still developing—especially important when deciding whether to prescribe medications and which ones. Certain conditions respond to medications, like severe depression, bipolar disorder, and ADHD. Mood stabilizers, antidepressants, stimulants are examples of medications that help control the main symptoms of these disorders. The good news is that roughly 60% of kids with ADHD will eventually outgrow it. But those with bipolar disorder will continue to experience symptoms, which are likely to increase as they age. One of the most promising ways to differentiate between a diagnosis of bipolar disease and one of ADHD is using biomarkers. Dr. Zeni is conducting research that studies the genetics of ADHD. He is researching “pharmacogenetics,” which tracks how a person responds to medication based on his or her genetic markers. Dr. Zeni is researching a specific gene, referred to as BDNF, which generates a special protein that has appeared in higher levels in those youngsters with bipolar disorder. Based on his studies, it appears that measuring these biomarkers may provide a shortcut for helping early diagnosis and treatment of children with bipolar disorder, which has shown to respond best when discovered and treated as early as possible.
Am I aging faster than I should be?
The concept of “accelerated aging” was first introduced after researchers started studying biological markers of aging and realized that sometimes the age that is detected in the laboratory does not concur with the actual age of a person. By definition, the “chronological age” measures the time elapsed since birth. Accordingly, individuals born on the same day will share the same chronological age throughout life, regardless of lifestyle, disease, or health. In contrast, individuals of identical chronological age may have different “biological ages”, which reflect the decline in the function of tissues and the organism.
Of note, the problem is not to have your chronological and biological ages out of sync; the problem is when you have a biological age that is actually older than your chronological age (“premature aging”). The ultimate goal of our research is to find ways to prevent premature aging, since it may increase the risk for aging-related diseases and contribute to an early decline in physical function. Thankfully, several strategies that have been scientifically suggested to prevent accelerated aging to some extent, including caloric restriction [1], healthier eating habits, exercising, having a good night’s sleep, avoiding drugs, tobacco, and alcohol.
The fact that some medical conditions can contribute to accelerated aging is not really new to Medicine. Doctors have been aware of rare genetic disorders known to cause premature aging and shorten life expectancy for years. What is fairly novel is the fact that common chronic diseases can also contribute to accelerated aging mechanisms. For instance, there is evidence to suggest that this is the case for some types of cancer, cardiovascular disease, heart failure, diabetes, liver cirrhosis, among others. With the support from the UTHealth Consortium on Aging and of The University of Texas Houston Retiree Organization (UTHRO), the Translational Psychiatry Program has been studying how psychiatric disorders, specifically bipolar disorder, can also contribute to accelerated aging. We have evidence that some patients with bipolar disorder show features of accelerated biological aging compared to healthy people [2]. While this is something that’s not carved in stone, still needs to be replicated by other research groups, and may not be true for all patients, it emphasizes the importance of carefully thinking of anti-aging strategies for these patients.
As discussed before, we could all be taking the effort to maintain healthier eating habits, exercise, prevent smoking habits, etc, and according to our studies this may be particularly important for patients with chronic conditions, such as bipolar disorder. Overall, we should be mindful that our lifestyle choices may be contributing to our biological age, especially if we already have a pre-existing condition that may make us more vulnerable to accelerated aging mechanisms.
References
[1] Balasubramanian P, Howell PR, Anderson RM. Aging and Caloric Restriction Research: A Biological Perspective With Translational Potential. EBioMedicine. 2017;21:37-44.
[2] Fries GR, Bauer IE, Scaini G, Wu MJ, Kazimi IF, Valvassori SS, Zunta-Soares G, Walss-Bass C, Soares JC, Quevedo J. Accelerated epigenetic aging and mitochondrial DNA copy number in bipolar disorder. Transl Psychiatry. 2017;7(12):1283.
Gabriel R. Fries, PhD, is an Instructor in the Department of Psychiatry and Behavioral Sciences and a researcher in the Translational Psychiatry Program. His research focuses on the epigenetic basis of mood disorders, with a particular interest in bipolar disorder and molecular mechanisms of stress.
How mobile health technology may reduce caregiver burden
UTHealth researchers — including Jair Soares, MD, PhD, Thomas D. Meyer, PhD, and first author Rebecca Casarez, PhD, RN, — conducted a qualitative study to understand the role of mobile health technology (mHealth) in reducing caregiver burden and improving well-being in spouses of patients with bipolar disorder. Results from focus group and in-depth interviews showed that the mHealth device may be helpful in at least six areas: reduction of stressors, decreased social isolation, improving communication in the relationship between spouses, speaking with children about the illness, managing medications, and providing information on resources. The article, published in the Journal of Affective Disorders, concludes that mHealth may be a feasible, available, and cost-effective support tool for spouses and partners of individuals with bipolar disorder. Read more below.
https://www.ncbi.nlm.nih.gov/pubmed/30877862
Suicide in Teens
Despite best efforts in public health to reduce youth suicide, rates of teen suicides have increased by 24 percent in the past 20 years. Every year, over 2,000 adolescents die by suicide, making it the second leading cause of death among teens in the United States. For every completed suicide there are 100-200 attempts made by desperate adolescents. Unfortunately, these teens are at an increased risk of attempting suicide again, especially within three months of their first attempt.
Suicidal teens typically feel worthless, guilty, and hopeless, often viewing suicide as way to escape mental pain or a difficult situation. Common risk factors include conflict with peers and family, interpersonal loss or disappointment, academic difficulties, legal problems, and abuse or assault. Most adolescents contemplating suicide display several warning signs, such as making suicidal threats; talking about suicide and death more generally; writing suicide notes to friends and family or posting “goodbye” messages on social media; and researching ways to die. They also tend to withdraw from friends and family; lose interests in school, sports, and other hobbies; engage in self-harming behaviors like cutting; and use drugs or alcohol to numb their feelings. Teens contemplating suicide may stop caring about their appearance and hygiene; appear depressed or irritable; and experience changes in sleep, appetite, and activity level. Parents and teachers who notice these signs and intervene can help prevent a suicide attempt.
Treatments for adolescents experiencing suicidality is promising. Although few psychotherapy studies have demonstrated replicated efficacy, Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT) have demonstrated reductions in suicidal ideation and suicidal behavior in clinical trials. While both therapies strive to improve emotional well-being and daily functioning, CBT focuses on changing maladaptive thoughts and behaviors, whereas DBT combines elements of CBT with techniques for distress tolerance, acceptance, and mindfulness. The combination of CBT and antidepressants can help lead to greater reductions in suicidality than medication alone.
For emergency help, call 911 or the National Suicide Hotline (1-800- 273-8255), go to the nearest emergency room, or seek assistance at:
NeuroPsychiatric Center 1502 Taub Loop, Houston, TX 77030 713-970-7070, or
UTHealth Harris County Psychiatric Center 2800 S. MacGregor Way Houston, TX 77021 713-741-5000
To find a physician at UTHealth/UT Physicians, please call 1-888-4UT-DOCS.
Ana Ugueto, PhD, is an assistant professor in the Department of Psychiatry and Behavioral Sciences. She is a child psychologist, who is trained in Cognitive-Behavioral therapy (CBT) for anxiety, depression, trauma, and behavioral problems in children and adolescents. She currently works in the Child and Adolescent Unit at UTHealth Harris County Psychiatric Center (HCPC) where she provides psychological consultation services. She regularly conducts group and individual assessments and therapy in an inpatient setting. Ugueto also specializes in disseminating evidence-based treatments (EBTs) in the community.
Researchers have identified cognitive measures as markers of vulnerability to pediatric bipolar disorder!
Cognitive impairments are primary hallmarks symptoms of bipolar disorder (BD). Whether these deficits are markers of vulnerability or symptoms of the disease is still unclear. Led by Isabelle Bauer, PhD, this study used a component-wise gradient (CGB) machine learning algorithm to identify cognitive measures that could accurately differentiate pediatric BD, unaffected offspring of BD parents, and healthy controls. Results showed that alterations in processing speed and affective processing are markers of BD in pediatric populations. Read more below.
How genes may lead to psychiatric disorders
Psychiatric disorders, such as bipolar disorder, are known to have a high heritability and a strong genetic component. This is evidenced by studies showing a high clustering of these disorders within families, in which first-degree relatives of patients have a significantly higher risk of developing behavioral alterations than the rest of the population. However, differently from single gene diseases (in which the inheritance of a mutated gene from one or two parents is enough to cause the disease in the offspring), complex diseases, such as psychiatric disorders, are not that simple. These disorders are caused by multiple genes interacting not only with each other, but also with one’s lifetime experiences. In other words, a “genes by environment” interaction is normally required to trigger the onset of psychiatric disorders, making them harder to treat and to predict from genetic tests.
How genes can interact with our life experiences is an open question that scientists have been trying to understand for a long time. Different mechanisms have been proposed and tested in various populations, and it is known that the presence of some genetic alterations can make a person more ‘vulnerable’ (or less resilient) to the effects of some stressful situations. In other words, two individuals experiencing similar traumatic events may develop different behavioral outcomes based on their distinct genetic makeup. More recently, the effects of environmental experiences in modulating so-called ‘epigenetic’ mechanisms have been proposed as mediators of these interactions, as well. Epigenetic modifications can induce significant changes in our DNA without changing its sequence. Highly relevant to Psychiatry, these modifications have also been shown to be quite stable (meaning that epigenetic alterations induced during childhood, for instance after an early trauma, may last until adulthood in specific cases).
Interestingly, several recent studies have reported epigenetic alterations in psychiatric patients. Among other areas of investigation, our Department is focused on better understanding the epigenetics of psychiatric disorders by studying blood samples from volunteers and post-mortem brain tissues of deceased patients after consent from the next-of-kin. We hope that our studies will contribute to the identification of innovative biomarkers and clinically-relevant targets for the development of novel treatments.
Gabriel R. Fries, PhD, is Instructor in the Department of Psychiatry and Behavioral Sciences at UTHealth and a translational researcher in the field of biological psychiatry. His research focuses on the epigenetic basis of mood disorders, with a particular interest in bipolar disorder, suicide, and molecular mechanisms of stress. Dr. Fries’ studies use basic science and investigation of cells, (epi)genomes and clinical datasets to better understand disease mechanisms and transmission, with the ultimate goal of designing novel medications and improving the lives of patients.
Scientists discover changes in the brain’s cellular powerhouses of bipolar disorder patients
Led by João Luciano de Quevedo, MD, Ph.D., and Giselli Scaini, Ph.D., scientists in the Department of Psychiatry and Behavioral Sciences discover changes in the cellular powerhouses of bipolar disorder patients. Glitches in the structures that provide power to cells may contribute to the mood swings experienced by the nearly 6 million American adults with bipolar disorder, report scientists from The University of Texas Health Science Center at Houston (UTHealth) in the journal Neuropsychopharmacology. In this study, researchers compared the mitochondria of 25 healthy subjects to 31 with bipolar disorder. They found a link between the severity of bipolar disorder and issues with the mitochondria function. When the severity increased, the number of mitochondria problems rose as well. While conducting their study, the researchers identified factors contributing to the breakdown of the mitochondria. These findings suggest that alterations in the mitochondrial network may play a role in producing psychiatric symptoms and the decline in functional status. Studies like this are relevant because this information could be used to help develop new treatments for this disorder.
Bipolar Research Project Spotlight
Christian P. Zeni, M.D., Ph.D., assistant professor in the Department of Psychiatry and Behavioral Sciences, researches risk factors and characteristics of children who have parents with bipolar disorder. Dr. Zeni talks about looking into clinical characteristics that can tell us which children can develop bipolar disorder, or not, later in life. #ManyFacesofUTHealth #BehavioralHealth
Giving thanks by giving back
In this season of giving, please consider making a donation in support of bipolar disorder research as part of the #GivingTuesday movement - a national celebration of giving.
Be a part of something greater on this #GivingTuesday and help us to continue developing research that allows us to shine a light and strengthen the overall understanding of Bipolar Disorder, a commonly misunderstood condition.
Your gift will make an impact!
Together, we can make this possible!
Thank you for being a part of our incredible journey to bring Understanding Bipolar Disorder through Research project to life. We are excited to extend the campaign as we continue to raise funds for this meaningful cause throughout the year.
With your support we will be able to provide more studies that could clarify the relationship between biomarkers and brain alterations at different phases of the disease, providing knowledge of why some patients will develop a more severe and debilitating course and others do not.
Please continue to share our mission with family, friends and those in our community.
We are grateful for your support! Thank you!
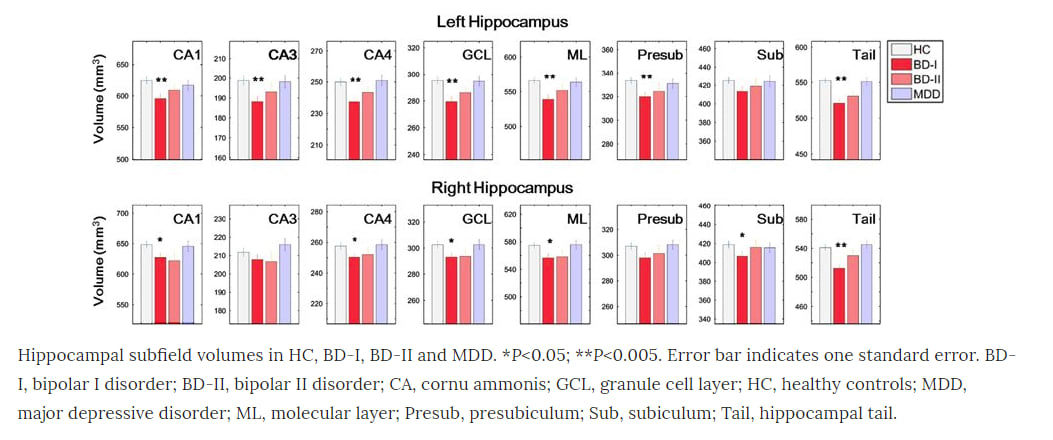
Researchers identify that children and adolescents with BD had smaller volumes in specific parts of the brain’s hippocampus
In line with the memory deficits observed in BD patients, hippocampal volume is heavily associated with several mood disorders and has been reported as a potential metric to diagnose and track progression of BD.
To investigate subfield volumes in the pediatric population, researchers at the UTHealth Center of Excellence on Mood Disorders acquired magnetic resonance imaging scans of 141 children and adolescents with bipolar disorder and major depressive disorder and healthy controls. Pediatric patients with bipolar disorder were found to have significantly smaller volumes in certain subfields of the hippocampus compared to healthy individuals, according to the study published in the Journal of Psychiatric Research. Results indicated deficits in the cornu ammonis (CA1 and CA4) and right subiculum, as well as the bilateral ganule cell layer, molecular layer and hippocampal tails.
Overall, the findings from this cross-sectional study provide evidence for specific hippocampal subfield volume differences in children and adolescents with BD compared to healthy controls, suggesting impaired neurogenesis and neural connectivity as well as progressive reductions with increased illness duration.
There is a lot more to be done! To help elucidate a causal relationship between illness duration and hippocampal subfield volumes, longitudinal studies must be conducted. Our ultimate goal is to find ways to prevent the onset of illness in these children and adolescents, and your help will help get there faster.
Researchers pinpoint area of brain linked to bipolar disorder
A volume decrease in specific parts of the brain’s hippocampus – long identified as a hub of mood and memory processing – was linked to bipolar disorder in a study led by our research group. The research was published in Molecular Psychiatry.
Our research team used a combination of magnetic resonance imaging (MRI) and a state-of-the-art segmentation approach to discover differences in the volumes of subfields of the hippocampus, a seahorse-shaped region in the brain. Subjects with bipolar disorder were compared to healthy subjects and subjects with major depressive disorder.
We found that subjects with bipolar disorder had reduced volumes in subfield 4 of the cornu ammonis (CA), two cellular layers and the tail portion of hippocampus. The reduction was more severe in patients with bipolar I disorder than other mood disorders investigated.
Further, in patients with bipolar I disorder, the volumes of certain areas such as the right CA1 decreased as the illness duration increased. Volumes of other CA areas and hippocampal tail were more reduced in subjects who had more manic episodes.
In conclusion, these results indicated that among the mood disorders the hippocampal subfields were more affected in BD-I compared with BD-II and MDD, and manic episodes had focused progressive effect on the CA2/3 and CA4 and hippocampal tail.
Please continue to share our mission with family, friends and those in our community.
We are grateful for your support! Thank you!
So excited to fill you in!
Thanks so much for supporting our campaign! You helped us raise 3,560.00 in 23 days! Your donation helped us reach our first key milestone in this campaign.
There are currently 22 days left in campaign and we still need to raise $21,440 of $25,000 that will allow us to study the relationship between biomarkers and alterations in the central nervous system in Bipolar Disorder patients.
Please remember that you can make a difference by sharing this important research with others. You will find buttons on our homepage that allows you to quickly and easily share to Facebook and Twitter. Together as a team, our efforts can help advance our understanding of bipolar disorder and improve the lives of patients.
Thank you for everything!
Impacting more lives with your help
According to our previous study published in Translational Psychiatry, a Nature Publishing Group journal, bipolar disorder may involve accelerated epigenetic aging, which could explain why persons with the disorder are more likely to have – and die from – age-related diseases.
While chronological age is measured in the amount of time a person has been alive, ‘epigenetic age’ measures molecular markers of chemical modifications to DNA. In this study we aimed to understand the biology of what is driving the accelerated aging in BD patients.
Using blood samples, our researchers compared 22 patients with bipolar disorder, 16 siblings of bipolar patients, and 20 healthy controls. Our results found that while older bipolar disorder patients had significantly accelerated epigenetic aging compared to controls, no difference was found in younger patients.
In addition, we also reported that patients present higher levels of mitochondrial DNA copy number, another marker of aging, and that this significantly correlated with the accelerated epigenetic aging. We believe that a difference was not detected in younger patients because they have not had as much exposure to stressful events, and this gave us a hint that the cumulative chronic exposure to stress would relate to accelerated aging.
Studies like this are important because they inform of the neurobiological basis of bipolar disorder and can provide targets for the development of novel and more efficacious treatments.
Thank you! We could not be doing this without you.
Despite advances in treatment options, many patients and families continue to struggle with the reality that even medications, short-term psychotherapies and inpatient treatments have not been enough to return some patients to full functioning. Our research aims to better understand bipolar disorder in order to improve the lives of patients.
We are 14 days into the campaign, and we are already at 11% of our $25,000 goal! Your support has been truly amazing!
Please continue to share our mission with family, friends and those in our community.
We are grateful for your support! Thank you!
Today is World Mental Health Day!
Today is a day dedicated to global mental health education, and it's time to look at mental illness from a different perspective – a positive one!
Let’s raise awareness of mental illness. Each of us can make a contribution to ensure that people dealing with problems concerning mental health can live better lives with dignity and respect.
Your support has the opportunity to touch countless lives as we strive to bring relief to patients with Bipolar Disorder and their families. Please take a moment to watch the following video about the research we undertake here, and help us spread the word by sharing our campaign with family and friends!
Let’s keep going!
Hey everybody!
Thanks for all of your support so far for this project! We are so grateful to everyone who has funded, shared and gotten involved.
We want to keep you posted on what we have accomplished so far:
We raised $2,345.00 since the campaign was launched!
There are 38 days left for this campaign and we still need to raise $22,655 of $25,000. Any amount will help support research on the mechanisms of bipolar disorder, leading to new biological targets for the development of innovative treatment.
Please also help us by sharing this important research on bipolar disorder with others. You will find buttons on our homepage that allows you to quickly and easily share to Facebook and Twitter. The more people learn about this important research, the more impact we can have.
Let’s keep going!
Thank you! We could not be doing this without you.
New Research Attempts to Explain Genetic Bipolar Disorder Connection
Thanks to everyone’s generous support! Here is one of the studies that we have done in our research program. Your kind help will allow us to develop more studies like this!
Genetic alterations that can be modulated by stress have been identified in children at high risk for bipolar disorder, according to our previous study published in Translational Psychiatry, a Nature Publishing Group journal.
Our research group analyzed peripheral blood mononuclear cells from a total of 18 children and adolescents in three matched groups: bipolar patients, unaffected offspring of bipolar parents and children of parents with no history of psychiatric disorders.
We have known that children of patients with bipolar disorder have a higher risk of developing the illness but the biological mechanisms are largely unknown, and by analyzing the blood of children of controls and comparing it to children of bipolar patients, we identified several genes or markers that can explain the increased risk. Moreover, the analysis revealed that, compared to children in the control group, bipolar patients and unaffected offspring of bipolar parents had genetic alterations that can influence the response to stress.
We know from clinical studies of behavior and the environment that when children are chronically exposed to stressors, they are at a higher risk of developing bipolar disorder. Bipolar parents may struggle because of their disease, leading to higher environmental stress. Their children, because of the genetic markers they have, could be more vulnerable to stress.
There is a lot more to be done! Our ultimate goal is to find ways to prevent the onset of illness in these children and adolescents, and your help will help get there faster.
Please continue to share our mission with family, friends and those in our community.
Thank you!

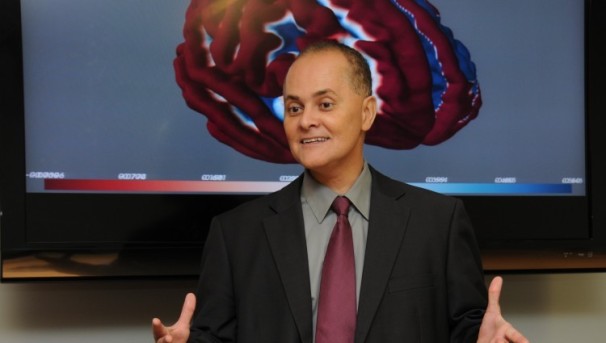
Our campaign is live!
We are excited to announce the launch of our campaign in support of bipolar disorder research. Our research is conducted at the UTHealth Center for Excellence on Mood Disorders, which is comprised of an active research team specializing in clinical neurosciences, as well as clinical psychopharmacology and interventions research. Led by our director, Jair C. Soares, M.D., Ph.D., professor and Pat R. Rutherford Jr. Chair in Psychiatry, our team has been studying bipolar disorder for a combined 25 of years. Our work has resulted in several groundbreaking findings that show exciting promise for future clinical applications.
Your generous gift will enable us to continue and increase the impact of our research, providing hope for patients, their families and our communities. A contribution in any amount makes a difference.
Please also remember to share our mission with family, friends and those in our community. Your support and involvement are greatly appreciated!